Donor Strip Harvesting to Meet Your Hair Restoration Needs
The great majority of patients who choose strip harvesting heal uneventfully with a narrow, easy to camouflage scar. Most patients are able to wear short hair without detectability issues.

While most prospective patients are aware that a linear scar will result from traditional donor site harvesting, few understand the mechanics of the donor site incision.
DONOR AREA BASICS
The first phase of the grafting process begins with the removal of a strip from the back and/or sides of the scalp. This process is referred to as "strip harvesting". The strip is removed from this area because hair in the donor region is resistant to the ravages of male pattern hair loss. The size of the donor strip is determined by several factors including: 1) the number of grafts being performed; 2) the follicular unit density in the donor region; and 3) the baseline elasticity of the donor scalp. It is easy to appreciate that larger graft sessions necessitate the removal of a larger strip.
DETERMINING STRIP SIZE
The strip dimensions are primarily influenced by the baseline follicular unit density and the scalp elasticity. Patients with high density hair will require a smaller strip than someone with low density hair. It is important to understand that follicular unit density can vary widely from person to person and it can also vary on any individual scalp from one location to another. Most patients have their highest density in the back of the scalp. Hair density in the back of the scalp typically ranges from 60-100 follicular units per square centimeter. It is quite common to find a lower hair density in the side regions of the scalp. Density in this area usually ranges from 50-80 follicular units per square centimeter and occasionally it is so low that a donor harvest may not be possible. Follicular unit density is measured with high-power magnification immediately prior to surgery in order to determine the precise size of strip that will be needed to provide the appropriate number of grafts for the restoration.
STRIP SIZE - DENSITY
Strip sizes can vary widely from person to person depending on their baseline hair density and elasticity. Consider three individuals who each require 2400 grafts. Patient A has 100 follicular units per square centimeter (high density hair); patient B has 80 follicular units per square centimeter (average density hair); and patient C has 60 follicular units per square centimeter (low-average density hair). Patient A will require a 24 square centimeter strip, patient B will require a 30 square centimeter strip and patient C will require a 40 square centimeter strip in order to provide the 2400 grafts needed for their respective procedures. The length of the final incision line if each patient were to have a 2 centimeter wide strip removed would be 12 centimeters for patient A, 15 centimeters for patient B and 20 centimeters for patient C. One can appreciate the donor "savings" that come with a high baseline hair density.
STRIP SIZE - ELASTICITY
Elasticity is the other factor that determines the length of the donor incision. An important point here is to appreciate that tension can adversely affect healing along the incision line. It is extremely important to limit tension on the final incision line closure so as to minimize visibility of the resulting scar. Similar to hair density, scalp elasticity can vary widely from person to person and from location to location. Some patients are fortunate to have a very loose scalp while others are limited by a tight donor area. Patients with a loose scalp can safely have a wider strip removed so as to produce a shorter strip and thereby a shorter donor scar. A tight scalp, comparable to the skin of an orange, necessitates the removal of a narrow strip in order to minimize tension along the incision line. Poor scalp elasticity requires a longer strip to compensate for the narrow width that is needed to allow a tension-free closure.
THE DONOR SCAR: INFLUENCES AND CARE
The final appearance of the donor scar will be influenced by three key factors: 1) the surgical technique; 2) intrinsic healing and physical properties; and 3) how the incision is managed by the patient during the various phases of healing. A deficiency in any one of these areas can lead to a less than ideal scar even if the other two factors transpire flawlessly. It is extremely important to understand that you will have a vital role in assuring the best result possible.
Surgical Factors
The road to a good donor scar begins with the technical expertise the surgeon. A perfect strip harvest requires a meticulous incision that parallels each follicle along the upper and lower edges of the strip. Because adjacent follicles are not perfectly aligned, the surgeon must constantly adjust the angle of the incision line cut in order to prevent follicular injury. High-power magnification and meticulous technique are required to assure the highest quality strip possible.
Once the strip is removed, the final closure will also affect the end result. Issues to consider here include: 1) layered versus non-layered closure; 2) trichophytic versus standard closure; and 3) staples versus sutures. In general, a layered closure is preferred over a non-layered closure because it helps to minimize tension along the scarline. A trichophytic technique is a modification of the incision closure which buries a row of follicular units into the incision line. The goal here is for the "buried" follicles to eventually grow through the overlying scar so as to help camouflage the final scarline. Finally, the decision between using staples or sutures will be made so as to provide the best long-term result for your scarline.
Intrinsic Factors
Scar healing can vary from person to person and it can vary from location to location in any given individual. The final scar will be influenced by your individual healing and physical characteristics. In general, the scalp tends to be a favorable zone for acceptable healing, but younger patients and patients with tighter skin may be at risk for a more detectable scar. Some patients heal with a more detectable scar despite a flawless surgical technique simply because of a deficiency in their own intrinsic healing properties. An experienced surgeon will be able to categorize your skin type and determine your risk for developing a less than ideal scar, in which case FUE can be considered for graft harvesting.
Your physical characteristics will also greatly influence the final detectability of your scar. Patients with longer hair, wavy hair, higher density hair and favorable hair/skin color combinations are best able to camouflage the donor incision with little difficultly. Hair length is usually the single most important limiting factor for adequate scar camouflage. Hair short enough to create a see-through effect to the scalp skin is too short to camouflage an average scar. Imagine having a tattoo on your scalp - if your hair is long enough to hide the tattoo then you will have no problem with scarline detectability. Patients who prefer a shaved scalp should not undergo a strip harvest procedure.
Patient Care Factors
The final factor that affects incision line healing is how you care for yourself during the healing process. Your incision will progress through several stages during the healing process which can be broken down into three main phases: 1) early; 2) intermediate; and 3) late.
Early Phase Healing
The early phase of healing begins on the day of surgery and ends about 2 weeks later. During this phase your incision will be held together by staples or sutures.
Intermediate Phase Healing
The intermediate phase lasts about 2-3 months and begins on the day your sutures or staples are removed. Scar tissue produced by your body during the early healing phase is weak and the immature scar tissue which holds the edges together at this time will be susceptible to stretching until it reaches full maturity a few months later. The most important factor to monitor during the intermediate phase is scar width. A "good" scar measures no more than 1-2 mm in width. Any tendency for a scar to widen beyond this is usually appreciated during the intermediate phase. The risk of widening increases with anything that "pulls" the incision line apart. Motions that compress the incision line are safe and those that stretch the incision line risk widening. Limiting neck flexion during the intermediate healing phase will help minimize the risk of widening. Fortunately, widening is uncommon following excellent surgical technique and proper patient self-care.
Late Phase Healing
The late phase of healing begins about 2-3 months after surgery and extends for about one year from the procedure. The scar at this time will lose its pink color - a sign that the incision is strong and will resist any further tendency to stretch.
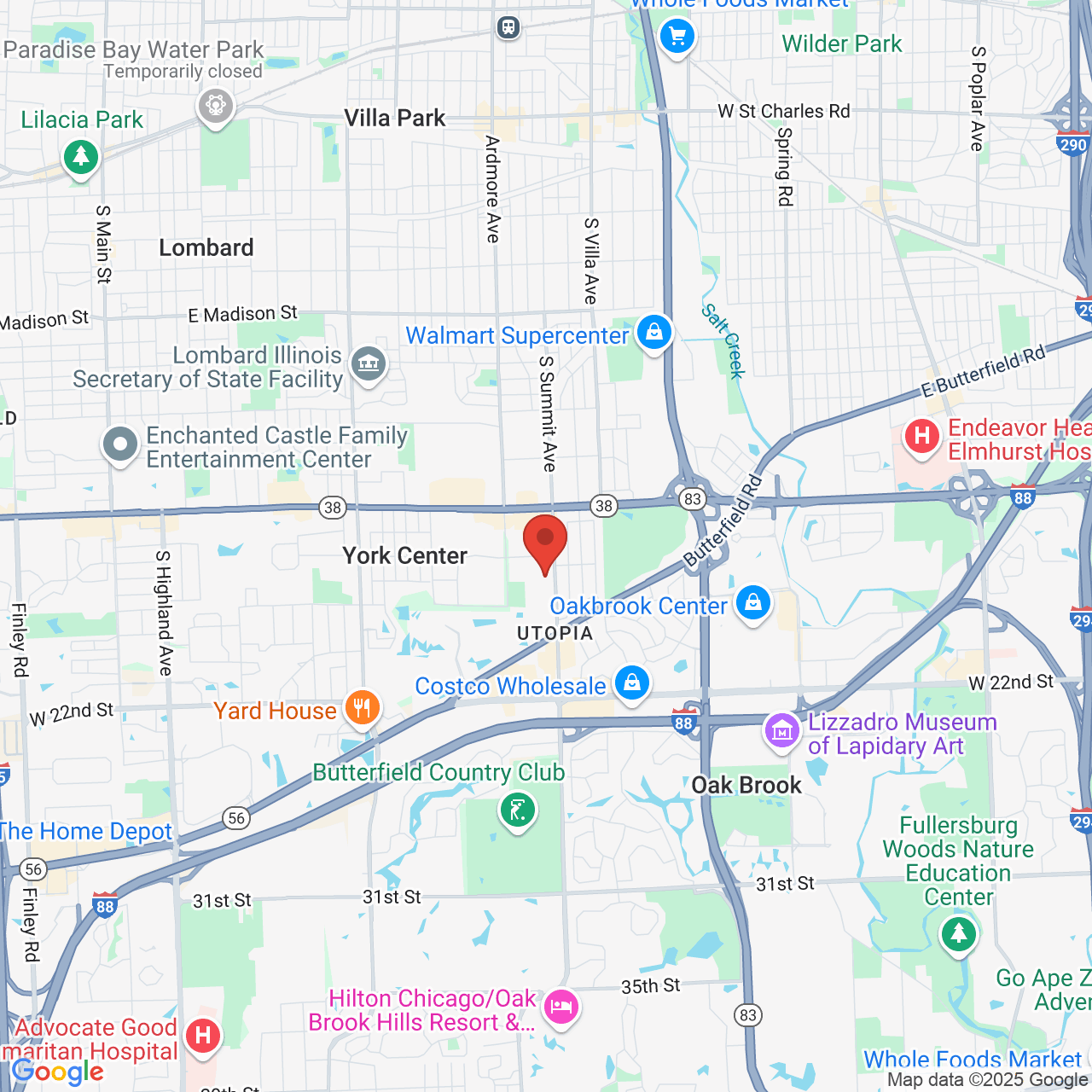
To contact our Oakbrook Terrace hair restoration office for a preliminary assessment of your hair loss, complete the virtual consultation form or call us at 630-932-9690.